Dementia is a generic term that refers to a number of different illnesses.
The most well known forms of dementia include Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease.
But Lewy Body Dementia?
Most people have never heard of it.
Yet Lewy Body Dementia, also called Dementia with Lewy Bodies (DLB) affects more than 1.4 million Americans and their families. That makes it the second most common form of dementia (behind Alzheimer’s).
In this article we’ll take a look at Lewy Body Dementia… what it is, what its symptoms are, and how to best care for a loved one with DLB.
What Is Lewy Body Dementia?
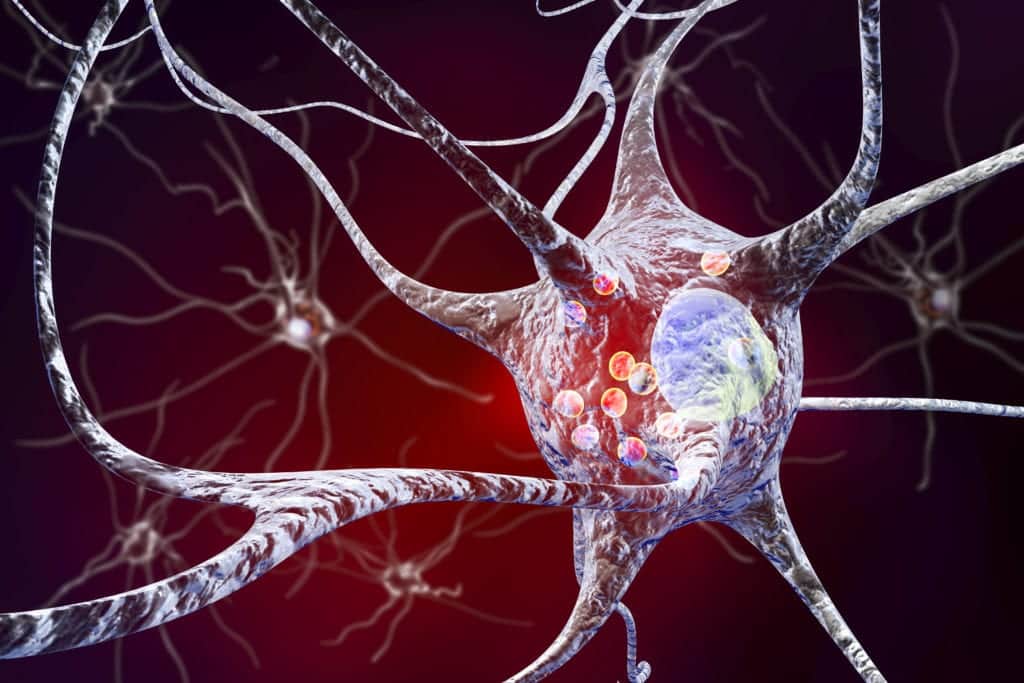
Lewy Body dementia is named after Lewy bodies. These are smooth, round clumps of protein that are located in nerve cells in the affected parts of the brain.
Lewy Body Dementia is relatively unique compared to other forms of dementia. That said, those with DLB may show many of the common dementia symptoms such as memory loss, confusion and agitation.
However, there are some important differences. And these differences effect the way the disease is diagnosed and managed.
How Is Lewy Body Dementia Different?
Lewy Body Dementia is a multi-system disease that affects things like thinking, movement and emotions.
When it comes to diagnosis, symptoms and outcomes, DLB is most like Parkinson’s disease.
There is no way to prevent or cure for either. They can share some similar symptoms. And sadly, both these forms of dementia ultimately result in death.
That said, there are key differences between Lewy Body, Parkinson’s and other forms of dementia. And understanding these differences are helpful for improving management of the disease and the affected person’s quality of life.
3 Key Differences Between Lewy Body Dementia and Other Forms of Dementia
1. You may know that tremors, muscle rigidity and changes in speech and walking are common in Parkinson’s. However, these symptoms may not be present in those with DLB. In fact, those with DLB often do not have the severe physical debilitation those with Parkinson’s experience.
Patients with Lewy Body Disease generally present more neuropsychiatric symptoms that distinguish the disease. Things like behavioral problems and visual hallucinations.Remember the Lewy bodies we mentioned earlier? Those lumps of proteins in nerve cells in the brain? Well, these proteins are common in those with other forms of dementia like Parkinson’s and Alzheimer’s too. However, not all of those patients will develop DLB.
2. Other forms of dementia tend to have more of a genetic component than Lewy Body Dementia. Huntington’s, for example, is considered a genetic disease.
3. That’s not the case with DLB. Yes, some families may have a genetic mutation that could increase their risk of DLB. However, Lewy Body Dementia is not typically genetic.
Diagnosis of Lewy Body Dementia
Lewy Body Dementia is particularly hard to diagnose. One way doctors identify those with DLB is by the core symptoms a patients displays.
These core symptoms are:
- Ongoing visual hallucinations.
- Parkinson’s disease like symptoms.
- A sleep disorder where people act out their dreams while sleeping.
- Unpredictable and changing alertness and cognitive function (i.e. thinking).
At least two of these symptoms need to be present to come to a DLB diagnosis.
However, there are currently no blood or other medical tests that can definitively diagnose Lewy Body Dementia. So doctors have to use a combination of symptoms, tests and ruling out other conditions to come to a definitive DLB diagnosis.
Treatment of Lewy Body Dementia
As we said, there is no cure for DLB. And treatment can be challenging.
Doctors typically will treat the symptoms. Often relying on drugs used primarily for Alzheimer’s and Parkinson’s disease.
Non-drug therapies may also be helpful. For example, dementia patients tend to do better when they have a structured routine. Keeping the patient in a calm, soothing environment may help as well. There are also therapies like music therapy or reminiscence therapy that have positive impacts.
Advice for Family Caregivers
The progression of dementia, in whatever form it takes, can seem relentless.
And seeing a loved one struggle and deteriorate as dementia progresses is extremely difficult. Especially for spouses and adult children who take on the role of caregivers.
Here are a few tips on providing the best possible care for your loved one.
- Stay in close touch with your loved one’s medical team and any professional care staff.
- Pay attention to, and tell doctors/other caregivers about, even the smallest changes in symptoms.
- Monitor their medications closely. Seniors with dementia may have bad reactions to certain drugs. Or often forget to take their drugs.
- Keep a close eye on them to try to prevent injuries due to falls or other accidents.
- And, if this gets too overwhelming, don’t be afraid to get help from in-home care or a memory care facility. While your loved one may not love the idea of having a companion caregiver, their safety and well-being needs to come first.
Finding Professional Memory Care
In the later stages of dementia, it’s likely your loved one will need care 24/7/365.
And, after a dementia diagnosis, it’s never too early to start making future plans. In fact, it’s often better to do this early on when your loved one is still able to speak for themselves. This will give them the opportunity to have a say in how they wish to spend their remaining years.
This may involve in-home care, adult day care, assisted living and/or a finding a dedicated memory care facility. To find options in your area, you can search for local dementia care facilities here.